Authors
Mishra, Pranav Kumar, Final MBBS, Part 1 – Kasturba Medical College, Manipal, Manipal University, Manipal, Karnataka
Singh, Rohit, Associate Professor of ENT– Kasturba Medical College, Manipal, Manipal University, Manipal, Karnataka
Nayak, Deepak Ranjan, Professor of ENT and Unit 1 Head – Kasturba Medical College, Manipal, Manipal University, Manipal, Karnataka
Case Overview
Clinical Presentation
A 21-year-old, Hepatitis-B positive, Indian male referred from a tertiary-care center to Kasturba Hospital presents with watering and protrusion of right eye, nose block, rapid swelling over the left forehead, and diffuse headache. The patient was apparently asymptomatic 1.5 months prior when he experienced an onset of continuous watering right eye associated with redness and itching. The patient concurrently developed a sudden onset of nose block, associated with epistaxis 4-5 times daily. One-month prior, the right eye began protruding, without any diplopia or vision change. A forehead swelling appeared 20 days prior.
On examination, we noted bilateral inferior turbinate hypertrophy, right eye proptosis, and a left frontal sinus area swelling of 3.5x2cm. The swelling was firm, fused, non-mobile, non-pulsatile, not fixed to the overlying skin.
Imaging

The CT revealed a heterogeneously enhancing soft tissue density in the right frontal ethmoidal, and maxillary sinuses; right nasal cavity with extension into the right orbit, lateral globe displacement. Malignant etiology was suspected.
Surgical management and pathological diagnosis
ENT and Neurosurgery performed an anterior craniofacial resection of the mass with lateral rhinotomy approach under general anesthesia with universal precautions. Neurosurgery noted a breached dura and arachnoid mater, with in-tact pia before using bone and fascia lata for skull base reconstruction. Histopathological examination with immunohistochemistry was diagnosed as alveolar type of rhabdomyosarcoma with solid areas. The patient developed CSF rhinorrhea, fever, and CSF findings suggestive of meningitis. Patient was managed conservatively with injection antibiotics and discharged at request on post-op day 15.
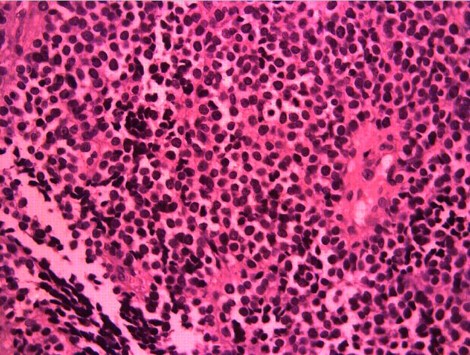
Rhabdomyosarcoma – alveolar type, with solid areas
- Monomorphic dyscohesive cells
- Scant cytoplasm, hyperchromic nuclei
- Occasional multinucleated giant cells
- Respiratory epithelium covering tumor stroma
- IHC: Desmin positive, Cytokeratin/LCA negative
Discussion
Rhabdomyosarcomas (RMS) are rare neoplasms in adulthood, often in unfavorable locations, of which alveolar histology accounts for only 14.5%1-3. This unusual case demonstrates the rapid invasiveness of RMS and risk for post-operative complications. Improved prognosis is associated with combined surgery, chemotherapy, and radiotherapy4. Socioeconomic and personal considerations factored in this case.
Case Presentation
With the support of wonderful faculty in the Department of ENT – Head and Neck Surgery at KMC, Manipal, I was able to win the 1st place award for “Oral Case Presentation”.
This case was presented at the Armed Forces Medical College, located in Pune, India. The panel of judges composed were composed of AFMC faculty, who are commissioned officers and physicians in India’s military. Organized by the AFMC Department of Internal Medicine, Illuminati is one of India’s leading national conferences for medical students.

References:
- Sultan I, Qaddoumi I, Yaser S, Rodriguez-galindo C, Ferrari A. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol. 2009;27(20):3391-7.
- Nakhleh RE, Swanson PE, Dehner LP. Juvenile (embryonal and alveolar) rhabdomyosarcoma of the head and neck in adults. A clinical, pathologic, and immunohistochemical study of 12 cases. Cancer. 1991;67(4):1019-24.
- Torres-peña JL, Ramos castrillo AI, Mencía-gutiérrez E, Gutiérrez-díaz E, Rodríguez-peralto JL, Bengoa-gonzález Á. Nasal Cavity or Alveolar Paranasal Sinus Rhabdomyosarcoma with Orbital Extension in Adults: 2 Cases. Plast Reconstr Surg Glob Open. 2015;3(6):e414.
- Seregard, Stefan. Management of alveolar rhabdomyosarcoma of the orbit. Acta Ophthalmologica Scandinavica. 80(6). Munksgaard International Publishers